经外周静脉置入中心静脉导管(peripherally inserted central venous catheter, PICC)广泛应用于新生儿重症监护病房(neonatal intensive care unit, NICU)的极低出生体质量儿(very low birth weight infant, VLBWI),主要是用来进行营养支持和药物的输送,由其导致的导管相关血流感染(catheter-related bloodstream infection, CRBSI)是最常见的医院感染,可导致新生儿住院时间延长、住院费用及病死率的增加;此外,VLBWI发生感染(早发性和晚发性败血症)后,幸存者5岁时出现不良神经发育结局的风险较高[1],因此,预防CRBSI具有重要的意义。为了明确VLBWI发生PICC CRBSI的危险因素并进行预防,本研究采用病例对照研究的方法对使用PICC的VLBWI的临床资料进行回顾性分析。
1 对象与方法 1.1 研究对象选取郑州大学第三附属医院2019年1月-2021年11月入住NICU的PICC置管VLBWI。纳入标准:①出生体质量<1 500 g(包括出生体质量<1 000 g的超低出生体质量儿);②出生0~28日龄;③在该院接受PICC穿刺术。排除标准:①存在产前感染及感染风险者;②置入PICC时间不足48 h。
1.2 研究方法采用病例对照研究的方法,以发生CRBSI者为病例组,未发生CRBSI者为对照组。CRBSI定义为带有血管内导管或者拔除导管48 h内,患者出现菌血症、伴有发热、寒战或低血压等感染表现,除血管导管外无其他明确感染源的感染性疾病[2]。制定统一调查记录表,记录所有新生儿的性别、胎龄、出生体质量、出生方式、有无新生儿窒息、有无机械通气、置管术穿刺部位、穿刺是否一次成功、置管时日龄、留置时间、清蛋白水平、血红蛋白水平及新生儿感染病原学结果等。
1.3 统计学方法应用SPSS 25.0软件对数据进行统计学分析。正态计量资料数据用均数±标准差(x±s)表示,采用t检验进行比较;不符合正态分布的计量资料采用M[P25, P75]表示;计数资料用例数或百分比表示,采用χ2检验进行比较;多因素分析采用logistic回归模型。P≤0.05为差异有统计学意义。
2 结果 2.1 一般情况及CRBSI发病率2019年1月-2021年11月,NICU留置PICC新生儿共1 073例,胎龄(29.9±2.4)周,PICC留置时间中位数20(13, 27)d,VLBWI 789例(包括超低出生体质量儿154例)。PICC新生儿中确诊CRBSI 62例(61例为VLBWI,1例为低出生体质量儿)。总置管时间26 521 d,CRBSI发病率为2.3‰。依据纳入排除标准最终纳入714例PICC新生儿,男性358例(50.1%)、女性356例(49.9%),胎龄(29.5±1.6)周,出生时体质量中位数1 170(1 020, 1 300)g;一次穿刺成功率为88.7%,PICC留置时间中位数21(15, 28)d。
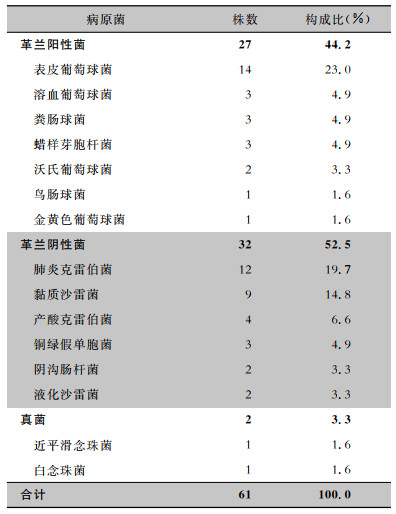
2.2 CRBSI病原菌分布61例发生CRBSI的VLBWI中,共分离出61株病原菌(排除污染情况),其中革兰阳性菌27株(44.2%);革兰阴性菌32株(52.5%);真菌2株(3.3%)。见表 1。
| 表 1 PICC置管VLBWI CRBSI病原菌分布 Table 1 Distribution of CRBSI pathogens in VLBWIs receiving PICC |
|
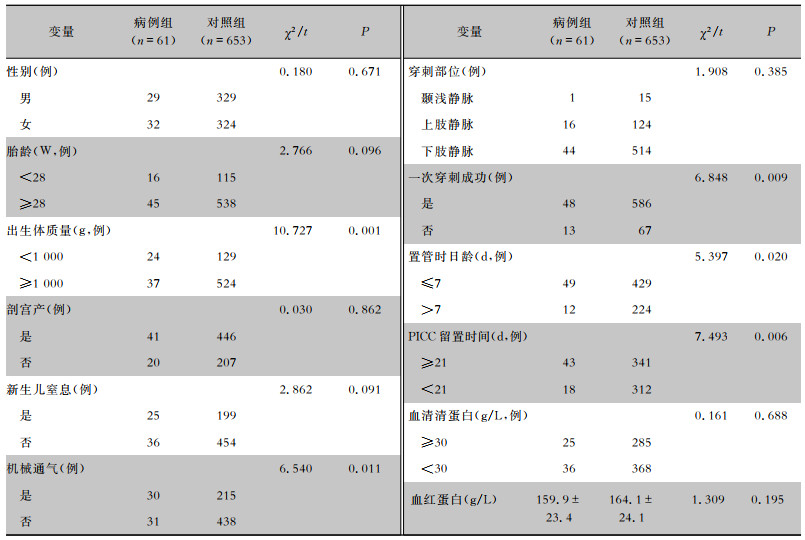
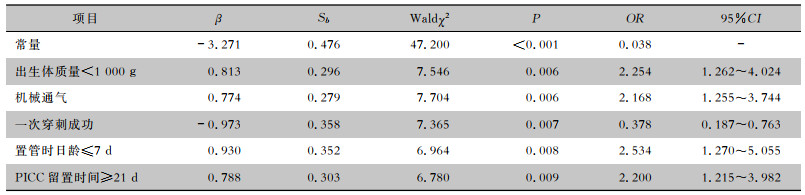
单因素分析发现,出生体质量<1 000 g、机械通气、未一次穿刺成功、置管时日龄≤7 d及PICC留置时间≥21 d VLBWI的CRBSI发病率较高,差异均有统计学意义(均P<0.05),见表 2。logistic回归分析表明,出生体质量<1 000 g(OR=2.254)、机械通气(OR=2.168)、置管时日龄≤7 d(OR=2.534)、PICC留置时间≥21 d(OR=2.200)是VLBWI发生CRBSI的独立危险因素,一次穿刺成功(OR=0.378)是保护性因素,见表 3。
| 表 2 PICC置管VLBWI发生CRBSI的单因素分析 Table 2 Univariate analysis on risk factors for CRBSI in VLBWIs receiving PICC |
|
| 表 3 PICC置管VLBWI发生CRBSI的多因素分析 Table 3 Multivariate analysis on risk factors for CRBSI in VLBWIs receiving PICC |
|
中心静脉置管导致的CRBSI在NICU的发病率最高[3-4],可达13.7‰[4],是国内外NICU长期面临的主要问题[5-6],特别是对于广泛接受PICC治疗的VLBWI[7],由于免疫系统不成熟,住院期间特别容易受到感染[8]。CRBSI可发生在置管数天或数周后,希腊的研究[9]发现,感染的新生儿较未感染的平均住院日长21 d,感染成本平均每例增加13 727欧元。本研究显示,CBRSI的病原菌大多为条件致病菌,最常见的是凝固酶阴性葡萄球菌(占31.1%),与国内外文献[3, 10-11]报道一致。已有研究[12]表明,凝固酶阴性葡萄球菌感染的减少可能会降低VLBWI认知障碍的发生率,临床工作中应对医疗护理质量持续改进,降低凝固酶阴性葡萄球菌的感染率和致残率。相较而言,真菌呈散发状态,不存在暴发流行,与于新颖等[13]的研究结果一致。
本研究显示,小胎龄被排除在VLBWI CRBSI的危险因素外,与诸多文献[13-15]报道不一致,根据中国新生儿重症监护室协作性质量改进研究协作组的调查[16]显示,新生儿CRBSI的发病率随胎龄的减小而升高,故对于PICC置管的小胎龄早产儿,我们仍不能放松对CRBSI的警惕性。此外,logistic回归分析显示,出生体质量低、PICC留置时间长可显著增加CRBSI发生的风险,与诸多文献[13-15, 17]报道结果一致。对VLBWI,尤其是超低出生体质量儿,喂养不耐受出现的概率较高,早期往往需要24 h输注静脉营养液,由于所使用的药物pH值和高渗透性会导致外周静脉出现液体渗出、化学性静脉炎、药液渗漏等并发症而拔管,外周静脉留置针保留时间多数在2~3 d,没有比PICC更安全的通道来进行中长时间的肠外营养治疗,但随着PICC留置时间的延长,细菌容易黏附在导管上并繁殖,CRBSI发生的概率亦随之上升,作为CRBSI发生的独立危险因素,PICC必须拔除的指征是新生儿出现感染的症状或体征,但必须更换的留置时间阈值尚未在文献中达成共识。对于临床医生而言,使用PICC之前,应充分考虑风险和收益,使用PICC之后,在对经外周中心静脉导管的管理中,对留置时间较长的新生儿,应每日评估是否有保留导管的必要,结束静脉营养治疗后应及时移除PICC,不可闲置在新生儿体内,一旦有临床感染症状或实验室感染依据,应尽早拔管。
本研究显示,机械通气是CRBSI的危险因素,与谢建宁等[18]的报道基本一致。机械通气作为一种侵入性操作,多应用于呼吸衰竭的VLBWI,人工气道的建立使气管直接向外,失去正常上呼吸道的过滤及非特异性免疫保护作用,如病房空气污浊,病原体可直接进入下呼吸道,细菌的黏附和定植随着机械通气时间的延长而增加,且机械通气下动脉血气分析、吸痰等有创操作难以避免,这些共同促进了新生儿CRBSI的发生。临床工作中,对机械通气的新生儿应严格无菌操作,并尽早撤机。
本研究显示,一次穿刺成功对CRBSI的发生有直接影响,与相关研究[19-20]结果一致,是CRBSI的保护性因素。若一次穿刺未成功,因血管细,管壁薄弱,会发生瘀青,需更改穿刺部位,再次消毒,增加了感染的机会,且反复穿刺会造成血管内壁和皮下组织大量的损伤,导致对微生物的防御能力降低,细菌容易侵入而发生CRBSI。
本研究还发现,置管时日龄较小是CRBSI发生的独立危险因素。原因考虑如下:早产儿皮肤结构尚未发育完善,角质层较薄,由2~3列角化细胞组成,角质层含有较少的保湿因子,皮肤保水能力比较差,经表皮水分丢失(transepidermal water loss, TEWL)较高,尤其在生后7 d内,早产儿的皮肤屏障相当脆弱,对于VLBWI或超低出生体质量儿,这个过程可能需要4周或更长的时间[21]。因此如在出生后早期进行侵入性操作,病原微生物更易侵入,成为全身感染的门户。
综上所述,VLBWI出生后早期不宜进行PICC操作,置管时避免反复穿刺,并尽量缩短PICC留置时间及机械通气时间,对于预防CRBSI具有重要意义。
利益冲突:所有作者均声明不存在利益冲突。
| [1] |
Mitha A, Foix-L'Hélias L, Arnaud C, et al. Neonatal infection and 5-year neurodevelopmental outcome of very preterm infants[J]. Pediatrics, 2013, 132(2): e372-e380. DOI:10.1542/peds.2012-3979 |
| [2] |
中华人民共和国国家卫生和计划生育委员会. 静脉治疗护理技术操作规范: WS/T 433-2013[S]. 北京: 中国标准出版社, 2014. National Health and Family Planning Commission of the People's Republic of China. Nursing practice standards for intravenous therapy: WS/T 433-2013[S]. Beijing: Standards Press of China, 2014. |
| [3] |
Broudic M, Bodet LM, Dumont R, et al. A 1-year survey of catheter-related infections in a pediatric university hospital: a prospective study[J]. Arch Pediatr, 2020, 27(2): 79-86. DOI:10.1016/j.arcped.2019.11.004 |
| [4] |
Carter JH, Langley JM, Kuhle S, et al. Risk factors for central venous catheter-associated bloodstream infection in pedia-tric patients: a cohort study[J]. Infect Control Hosp Epide-miol, 2016, 37(8): 939-945. DOI:10.1017/ice.2016.83 |
| [5] |
Wen J, Yu Q, Chen HY, et al. Peripherally inserted central venous catheter-associated complications exert negative effects on body weight gain in neonatal intensive care units[J]. Asia Pac J Clin Nutr, 2017, 26(1): 1-5. |
| [6] |
Yuan Y, Zhou W, Rong X, et al. Incidence and factors associa-ted with nosocomial infections in a neonatal intensive care unit (NICU) of an urban children's hospital in China[J]. Clin Exp Obstet Gynecol, 2015, 42(5): 619-628. DOI:10.12891/ceog1935.2015 |
| [7] |
吕倩, 陈茜, 徐敏, 等. 新生儿PICC相关血流感染的危险因素[J]. 中国感染控制杂志, 2019, 18(6): 587-589. Lv Q, Chen X, Xu M, et al. Peripherally inserted central catheter-related bloodstream infection in neonates[J]. Chinese Journal of Infection Control, 2019, 18(6): 587-589. |
| [8] |
Zingg W, Hopkins S, Gayet-Ageron A, et al. Health-care-associated infections in neonates, children, and adolescents: an analysis of paediatric data from the European Centre for Di-sease Prevention and Control point-prevalence survey[J]. Lancet Infect Dis, 2017, 17(4): 381-389. DOI:10.1016/S1473-3099(16)30517-5 |
| [9] |
Karagiannidou S, Zaoutis T, Maniadakis N, et al. Attributable length of stay and cost for pediatric and neonatal central line-associated bloodstream infections in Greece[J]. J Infect Public Health, 2019, 12(3): 372-379. DOI:10.1016/j.jiph.2018.12.004 |
| [10] |
庄秀娟, 霍开明, 徐莉, 等. 新生儿重症监护病房患儿经外周静脉置入中心静脉导管相关血流感染的病原菌分布及耐药性分析[J]. 中华医院感染学杂志, 2018, 28(7): 1097-1099, 1103. Zhuang XJ, Huo KM, Xu L, et al. Distribution and drug resistance of pathogens associated with peripherally inserted central catheter related bloodstream infections in neonatal intensive care unit[J]. Chinese Journal of Nosocomiology, 2018, 28(7): 1097-1099, 1103. |
| [11] |
Greenberg RG, Cochran KM, Smith PB, et al. Effect of cathe-ter dwell time on risk of central line-associated bloodstream infection in infants[J]. Pediatrics, 2015, 136(6): 1080-1086. DOI:10.1542/peds.2015-0573 |
| [12] |
Davis JW, Odd D, Jary S, et al. The impact of a sepsis quality improvement project on neurodisability rates in very low birthweight infants[J]. Arch Dis Child Fetal Neonatal Ed, 2016, 101(6): F562-F564. DOI:10.1136/archdischild-2015-309804 |
| [13] |
于新颖, 姜红, 范玲. 极低出生体质量儿PICC导管相关血流感染的危险因素及早期临床特点[J]. 中国医科大学学报, 2016, 45(10): 948-951. Yu XY, Jiang H, Fan L. Risk factors for PICC catheter-rela-ted blood stream infection in very low birth weight infants and the early clinical characteristics[J]. Journal of China Medical University, 2016, 45(10): 948-951. DOI:10.12007/j.issn.0258-4646.2016.10.021 |
| [14] |
庄秀娟, 霍开明, 徐莉, 等. 极低出生体质量儿PICC导管相关血流感染的影响因素及早期临床特点[J]. 中华医院感染学杂志, 2018, 28(15): 2372-2376. Zhuang XJ, Huo KM, Xu L, et al. Risk factors and early stage clinical features of PICC catheter-related bloodstream infections in very low birth weight infants[J]. Chinese Journal of Nosocomiology, 2018, 28(15): 2372-2376. |
| [15] |
帅春, 封志纯, 汪灏, 等. 极低出生体质量儿置入中心静脉导管相关血流感染的临床研究[J]. 临床儿科杂志, 2015, 33(1): 9-12. Shuai C, Feng ZC, Wang H, et al. Investigation of periphera-lly inserted central catheter-associated infection in very low birth weight infants[J]. Journal of Clinical Pediatrics, 2015, 33(1): 9-12. DOI:10.3969/j.issn.1000-3606.2015.01.003 |
| [16] |
中国新生儿重症监护室协作性质量改进研究协作组. 2015至2018年中国25家医院新生儿重症监护室早产儿中心导管相关性血流感染发生率的横断面调查[J]. 中国循证儿科杂志, 2019, 14(4): 241-246. Reduction of Infection in Neonatal Intensive Care Units using the Evidence-based Practice for Improving Quality (REIN-EPIQ) Study Group. A cross-sectional survey of the incidence of central line-associated bloodstream infections in preterm infants in NICUs of 25 hospitals in China from 2015 to 2018[J]. Chinese Journal of Evidence-Based Pediatrics, 2019, 14(4): 241-246. DOI:10.3969/j.issn.1673-5501.2019.04.001 |
| [17] |
张月沥, 周碧琼, 蒲林, 等. 新生儿PICC置管后血流感染相关因素分析及护理对策探讨[J]. 世界最新医学信息文摘, 2021, 21(41): 352-353. Zhang YL, Zhou BQ, Pu L, et al. Analysis of related factors and nursing countermeasures of bloodstream infection after PICC catheterization in newborns[J]. World Latest Medicine Information, 2021, 21(41): 352-353. |
| [18] |
谢建宁, 高平明, 黄朝梅, 等. 新生儿导管相关血流感染危险因素分析[J]. 实用医学杂志, 2018, 34(4): 618-620. Xie JN, Gao PM, Huang ZM, et al. Analysis of risk factors for catheter-related bloodstream infection in neonates[J]. The Journal of Practical Medicine, 2018, 34(4): 618-620. DOI:10.3969/j.issn.1006-5725.2018.04.023 |
| [19] |
先疆燕, 王荣丽, 何文英. 新生儿外周静脉置入中心静脉导管相关性感染危险因素的荟萃分析[J]. 中国感染与化疗杂志, 2020, 20(1): 27-31. Xian JY, Wang RL, He WY. Risk factors of peripherally inserted central catheter-related infections in neonates: a Meta-analysis[J]. Chinese Journal of Infection and Chemotherapy, 2020, 20(1): 27-31. |
| [20] |
周远珍. 经外周静脉穿刺中心静脉置管早产儿出现导管相关性血流感染的危险因素及护理对策[J]. 医疗装备, 2021, 34(13): 157-159. Zhou YZ. Risk factors of catheter-related bloodstream infection occurred in preterm infants caused by peripherally inserted central venous catheter and the nursing strategies[J]. Chinese Journal of Medical Device, 2021, 34(13): 157-159. DOI:10.3969/j.issn.1002-2376.2021.13.076 |
| [21] |
Kalia YN, Nonato LB, Lund CH, et al. Development of skin barrier function in premature infants[J]. J Invest Dermatol, 1998, 111(2): 320-326. DOI:10.1046/j.1523-1747.1998.00289.x |



