2. 济源市第三人民医院医院感染管理科,河南 济源 454650;
3. 郑州大学第一附属医院小儿内科,河南 郑州 450052
2. Department of Healthcare-associated Infection Management, The Third People's Hospital of Jiyuan City, Jiyuan 454650, China;
3. Department of Pedia-trics, The First Affiliated Hospital of Zhengzhou University, Zhengzhou 450052, China
急性白血病(acute leukemia)是儿童常见的恶性肿瘤之一,由于疾病自身特点及化学治疗(化疗)药物的应用,白血病患儿存在不同程度的免疫功能缺陷,较易导致医院感染的发生[1-2]。感染导致的脓毒症及脓毒性休克已成为儿童白血病长期的生存障碍之一[3]。本文在日常医院感染目标性监测的基础上,通过巢式病例对照研究,探讨急性白血病患儿化疗期间发生医院感染并发脓毒症的临床特点及其相关危险因素,以便为儿童急性白血病相关脓毒症的有效防控提供依据。
1 对象与方法 1.1 研究对象选取2021年1月—2022年6月某三级医院小儿内科急性白血病确诊患儿为研究对象,开展医院感染前瞻性监测。纳入标准:符合《实用小儿血液病学》[4]急性白血病的诊断标准;年龄1~14岁;无意识障碍,主要器官无严重功能障碍,病情稳定,无代谢性疾病;住院时长>48 h;住院期间实施化疗;征得患儿或监护人同意,监护人签署知情同意书。排除标准:急症患儿;有认知障碍、精神病史、无法进行正常语言交流且无监护人陪护者。
1.2 研究方法采用巢式病例对照研究方法,以监测期间临床诊断为脓毒症的急性白血病患儿为病例组,按照1∶2的比例,以住院时间(±7 d)为配对条件,随机选取未发生脓毒症、白血病类型相同的患儿为对照组,排除社区感染、使用抗菌药物,以及资料不完整的患儿。收集研究对象病原学及临床资料,包括年龄、性别、疾病危险度、白血病类型、既往住院情况和感染情况、化疗方案、骨髓移植、侵入性操作(手术、穿刺、留置导管)、糖皮质激素使用、层流床使用及入院时骨髓原始细胞比例、白细胞水平、中性粒细胞绝对值、血清清蛋白等指标。分析脓毒症病原体分布及药敏情况;比较两组患儿基本资料和研究指标的差异。随访所有纳入研究的患儿直至出现脓毒症、死亡等结局或研究时间终点(2022年6月30日)。病例诊断由医院感染管理专职人员和临床医生依据诊断标准、结合检验结果进行医院感染和脓毒症的判断。
1.3 诊断标准参照《中国脓毒症/脓毒性休克急诊治疗指南(2018)》[5],对于感染或疑似感染的患者,当脓毒症相关序贯器官衰竭[sequential(sepsis-related)organ failure assessment, SOFA]评分较基线上升≥2分,诊断为脓毒症。依据国家卫生部《医院感染诊断标准(试行)》[6]进行医院感染的判定。
1.4 血培养方法按照《临床微生物实验室血培养操作规范》WS/T 503—2017[7],疑似感染患儿均采集至少双套培养(2瓶需氧,必要时加厌氧,总采血量4~20 mL),留置静脉导管患儿同时抽取导管内和外周静脉血送检,未留置静脉导管患儿同时抽取双侧不同部位外周静脉血送检。
1.5 多重耐药菌定义指对临床使用的三类或三类以上抗菌药物同时呈现耐药的细菌[8]。
1.6 统计学方法应用SPSS 24.0统计学软件进行数据处理。符合正态分布的计量资料以均数±标准差(x±s)表示,两组独立、正态、方差齐资料的组间比较采用t检验;计数资料采用频数、百分比表示,组间比较采用χ2检验或Fisher确切概率法;多因素分析采用非条件二元logistic回归分析法。以P≤0.05表示差异具有统计学意义。
2 结果 2.1 患儿基本情况研究期间,共有1 023例急性白血病患儿在该科住院治疗,排除未实施化疗患儿160例、未同意参与调查患儿29例、急症患儿15例,最终有819例急性白血病患儿符合要求纳入本研究。819例患儿中,发生脓毒症51例,发病率为6.23%。其中,男性27例(52.94%),女性24例(47.06%);平均年龄(8.41±4.11)岁;急性淋巴细胞白血病35例(68.63%)、急性髓系白血病16例(31.37%);46例(90.20%)感染部位明确者,分别为血液29例(56.86%),呼吸道15例(29.42%),肛周及皮肤各1例(分别占2.00%),未明确感染部位者5例(9.80%)。
以监测期间临床诊断为脓毒症的51例急性白血病患儿为病例组,按照配对条件选取102例患儿为对照组。
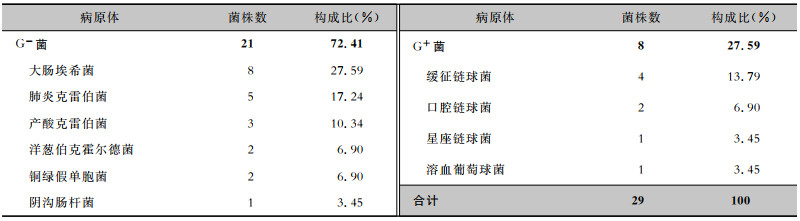
2.2 病原体分布51例急性白血病脓毒症患儿血标本共检出病原体29株。其中革兰阴性(G-)菌21株(72.41%),革兰阳性(G+)菌8株(27.59%)。G-菌以大肠埃希菌(27.59%)、肺炎克雷伯菌(17.24%)居多;G+菌以链球菌为主,以缓征链球菌(13.79%)居多。见表 1。
| 表 1 儿童急性白血病脓毒症血标本病原体分布 Table 1 Distribution of pathogens from blood specimens of acute leukemia children complicated with sepsis |
|
检出G-菌中,肠杆菌目细菌(大肠埃希菌及肺炎克雷伯菌)未发现对替加环素、黏菌素耐药的菌株。大肠埃希菌对氨苄西林、头孢呋辛、环丙沙星、左氧氟沙星、多西环素的耐药率>80%;肺炎克雷伯菌对氨苄西林、头孢唑林、妥布霉素、环丙沙星、多西环素、米诺环素、复方磺胺甲
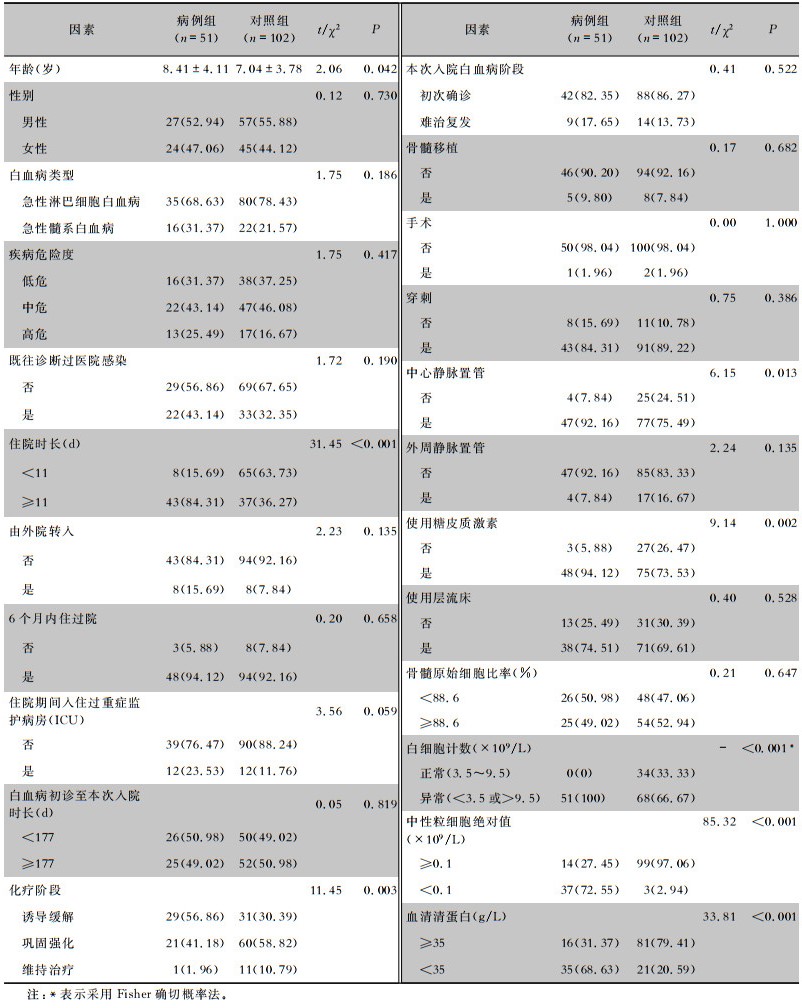
病例组与对照组在年龄、住院时长、化疗阶段、中心静脉置管、使用糖皮质激素、白细胞计数、中性粒细胞绝对值、血清清蛋白水平方面比较,差异均有统计学意义(均P<0.05)。见表 2。
| 表 2 儿童急性白血病合并脓毒症影响因素的单因素分析 Table 2 Univariate analysis on influencing factors for acute leukemia children complicated with sepsis |
|
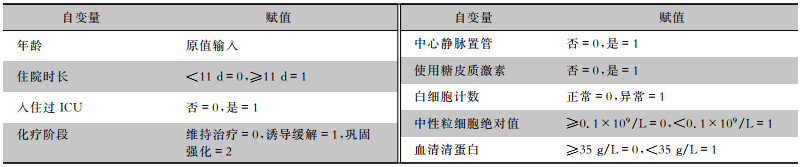
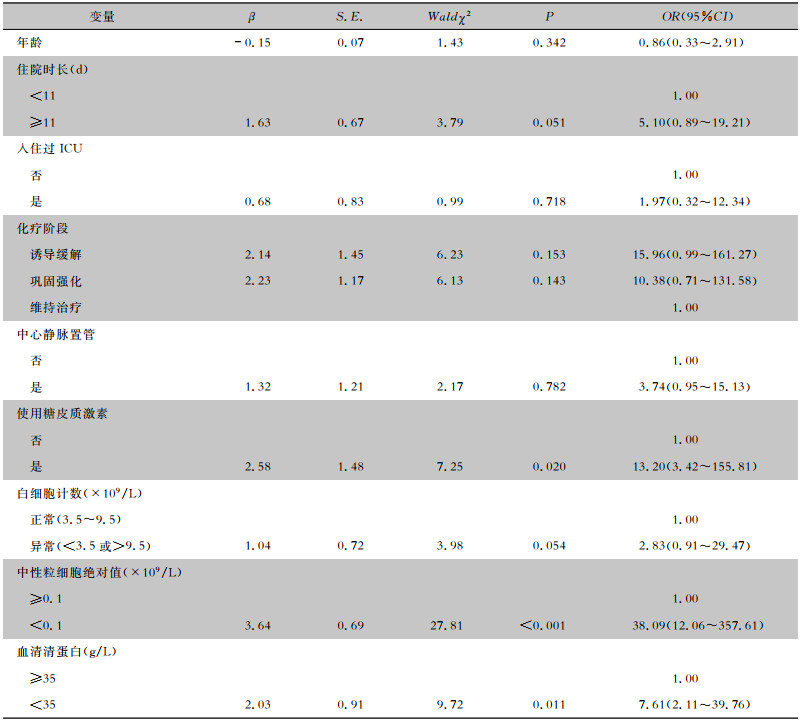
将急性白血病儿童是否发生脓毒症作为因变量,对单因素分析中有统计学差异或临界的因素进行赋值,见表 3。二元logistic多因素回归分析结果显示,按年龄进行调整后,使用糖皮质激素(OR=13.20,95%CI: 3.42~155.81)、中性粒细胞绝对值< 0.1×109/L(OR=38.09,95%CI: 12.06~357.61)、血清清蛋白<35 g/L(OR=7.61,95%CI: 2.11~39.76)为急性白血病儿童化疗期间发生脓毒症的独立危险因素(均P<0.05),见表 4。
| 表 3 儿童急性白血病合并脓毒症危险因素的变量赋值 Table 3 Variable assignment of risk factors for acute leukemia children complicated with sepsis |
|
| 表 4 儿童急性白血病合并脓毒症危险因素的多因素分析 Table 4 Multivariate analysis on risk factors for acute leukemia children complicated with sepsis |
|
脓毒症是儿童急性白血病化疗期间常见合并症之一,极易造成患儿预后不佳。本研究发现,急性白血病患儿化疗期间医院感染导致的脓毒症发病率达到6.23%;近年来文献[9-10]报道儿童急性白血病合并脓毒症发病率也维持在较高水平。一旦造成脓毒症或脓毒性休克,则大大增加了死亡风险[11]。因此,在急性白血病患儿化疗期间,应注重医院感染及脓毒症的监测,分析危险因素,以利于早期、个体化干预。
本研究发现,儿童急性白血病脓毒症血标本病原体以大肠埃希菌、肺炎克雷伯菌等肠杆菌为主,与文献[12]报道一致。这可能是由于化疗过程中口腔和下呼吸道的微生物通过炎症病变的黏膜转移到血液中而造成[13]。因此,化疗期间应重视患者黏膜保护,加强口腔护理[14]。另外,本研究发现脓毒症相关病原体均为多重耐药菌。所以,在临床诊疗、护理中,应采取一系列措施,如提高医务人员手卫生依从性,严格落实接触隔离措施,规范合理使用抗菌药物,以有效控制多重耐药菌在急性白血病患儿中的传播[15-16]。
本研究中,化疗诱导缓解期发生脓毒症的概率相对维持治疗期较高,可能与该阶段白血病细胞大量浸润导致机体抵抗力下降,加之糖皮质激素持续使用引发严重骨髓抑制和粒细胞缺乏等有关[17],提示该时期可能是脓毒症的高发阶段。另外,与未留置中心静脉导管急性白血病患儿相比,留置该类型导管患儿脓毒症的发病率明显升高,与其他文献[9, 18]报道的结果一致。因此,应密切观察患儿感染征象,规范血管导管置管和维护操作,预防感染发生[19]。
多因素分析结果显示,中性粒细胞绝对值<0.1×109/L的急性白血病患儿发生脓毒症的风险更高。以往研究中,中性粒细胞绝对值低于0.1×109/L且粒细胞缺乏持续时间超过7 d被认为是脓毒症发生的高危因素[20]。由于中性粒细胞产生于骨髓造血细胞,具有免疫作用,一旦缺乏,则较易引发医院感染[21]。急性白血病患者本身骨髓造血功能有缺陷,中性粒细胞的数量和质量均较低;化疗又会进一步影响骨髓造血功能,导致中性粒细胞数量、质量及其功能恶化,机体将难以对抗致病菌侵袭而易诱发感染[22-23]。因此,建议在患儿化疗后,可根据中性粒细胞水平或缺乏持续时间,积极预防性抗感染治疗及粒细胞集落刺激因子的支持治疗[9]。
急性白血病患儿在化疗诱导缓解期间,常使用左旋门冬酰胺酶;为避免该药引起的胰腺炎,临床往往建议6周内低脂饮食,但这有可能导致营养不良[24]。一般而言,患者营养状况越差,发生医院感染的风险越高[25-26]。本研究中,血清清蛋白低于35 g/L是急性白血病患儿发生脓毒症的独立危险因素,与其他报道结论一致[27-28]。这可能与清蛋白水平降低会使机体正常酶的数量和活性下降,造成机体免疫力降低,增加感染风险有关[29]。因此,建议尽早给与急性白血病患儿营养支持,尽快改善其营养状况,以预防医院感染。
糖皮质激素,如地塞米松或泼尼松等,除杀灭肿瘤细胞之外,还将抑制免疫应答,破坏淋巴细胞和干扰补体参与免疫反应,从而引发感染[30-32]。本研究中,糖皮质激素的使用可能会明显增加急性白血病患儿发生脓毒症的风险。因此,建议应关注急性白血病患儿糖皮质激素的规范应用,加强日常护理,树立安全注射意识,以降低外源性感染的发生风险。
综上所述,应加强急性白血病患儿化疗期间,特别是诱导缓解期的监测与随访,密切关注留置中心静脉导管、使用糖皮质激素治疗、中性粒细胞绝对值和血清清蛋白水平较低的患儿;病区的管理中,注重各项感染防控措施的有效落实,强化无菌观念,加强环境的清洁与消毒、医务人员手卫生等,落实急性白血病患儿的保护性隔离措施,尽量缩短住院时长,有效阻断多重耐药菌的传播等,从而减少医院感染导致的脓毒症发生。
利益冲突:所有作者均声明不存在利益冲突。
| [1] |
姚佳峰, 李楠, 姜锦. 单中心血液肿瘤患儿合并感染病原菌分布及耐药性病例系列报告[J]. 中国循证儿科杂志, 2019, 14(2): 112-117. Yao JF, Li N, Jiang J. Prevalence and drug-resisitance of pathogenic organisms in pediatric hematology and oncology department: a single center retrospective study[J]. Chinese Journal of Evidence Based Pediatrics, 2019, 14(2): 112-117. |
| [2] |
Freifeld AG, Bow EJ, Sepkowitz KA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America[J]. Clin Infect Dis, 2011, 52(4): 427-431. DOI:10.1093/cid/ciq147 |
| [3] |
Xiao CX, Wang S, Fang F, et al. Epidemiology of pediatric severe sepsis in main PICU centers in southwest China[J]. Pediatr Crit Care Med, 2019, 20(12): 1118-1125. DOI:10.1097/PCC.0000000000002079 |
| [4] |
黄绍良, 陈纯, 周敦华. 实用小儿血液病学[M]. 北京: 人民卫生出版社, 2014. Huang SL, Chen C, Zhou DH. Practical pediatric hematology[M]. Beijing: People's Medical Publishing House, 2014. |
| [5] |
中国医师协会急诊医师分会, 中国研究型医院学会休克与脓毒症专业委员会. 中国脓毒症/脓毒性休克急诊治疗指南(2018)[J]. 感染、炎症、修复, 2019, 20(1): 3-22. Emergency Physicians Association of Chinese Medical Doctor Association, Professional Committee on shock and sepsis of Chinese Research Hospital Association. Emergency treatment guidelines for sepsis/septic shock in China (2018)[J]. Infection Inflammation Repair, 2019, 20(1): 3-22. |
| [6] |
中华人民共和国卫生部. 医院感染诊断标准(试行)[J]. 中华医学杂志, 2001, 81(5): 314-320. Ministry of Health, PRC. Diagnostic criteria for nosocomial infections(proposed)[J]. National Medical Journal of China, 2001, 81(5): 314-320. |
| [7] |
中华人民共和国国家卫生和计划生育委员会. 临床微生物实验室血培养操作规范: WS/T 503—2017[S]. 北京: 中国标准出版社, 2017. National Health and Family Planning Commission of the People's Republic of China. Operating procedures of blood culture for clinical microbiology laboratory: WS/T 503-2017[S]. Beijing: Standards Press of China, 2017. |
| [8] |
中华人民共和国国家卫生健康委员会医政司. 卫生部办公厅关于印发《多重耐药菌医院感染预防与控制技术指南(试行)》的通知: 卫办医政发〔2011〕5号[EB/OL]. (2011-01-26)[2023-01-25]. http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=50487. Department of Medical Affairs of the State Health Commission of the National Health Commission. Notice of the General Office of the Ministry of Health on the Issuance of the "technical guidelines for the prevention and control of multidrug resistant bacterial hospital infections (trial)": Health Office Medical Issuing[2011] No. 5[EB/OL]. (2011-01-26)[2023-01-25]. http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=50487. |
| [9] |
张晓晓, 管贤敏, 宪莹, 等. 儿童急性淋巴细胞白血病化疗后并发脓毒症临床分析[J]. 临床儿科杂志, 2016, 34(11): 853-856. Zhang XX, Guan XM, Xian Y, et al. Clinical characteristics of septicemia with positive blood cultures episodes in pediatric acute lymphoblastic leukemia patients after chemotherapy[J]. Journal of Clinical Pediatrics, 2016, 34(11): 853-856. DOI:10.3969/j.issn.1000-3606.2016.11.013 |
| [10] |
Ammann RA, Laws HJ, Schrey D, et al. Increased risk of severe sepsis in Hispanic children hospitalized with acute myeloid leukemia[J]. Eur J Pediatr, 2015, 174(5): 675-686. DOI:10.1007/s00431-015-2525-5 |
| [11] |
陈雪婷, 钱素云. 全球儿童脓毒症流行病学及病原学研究进展[J]. 中华儿科杂志, 2019, 57(5): 380-383. Chen XT, Qian SY. Progress in epidemiology and etiology of pediatric sepsis[J]. Chinese Journal of Pediatrics, 2019, 57(5): 380-383. DOI:10.3760/cma.j.issn.0578-1310.2019.05.014 |
| [12] |
郑湧智, 李健, 乐少华, 等. 恶性血液病儿童化疗后合并血流感染的病原菌分布及耐药情况分析[J]. 中华血液学杂志, 2019, 40(3): 235-237. Zheng YZ, Li J, Yue SH, et al. Bacterial distribution and drug resistance of pathogens of blood stream infection in children with hematological malignancies after chemotherapy[J]. Chinese Journal of Hematology, 2019, 40(3): 235-237. |
| [13] |
任媛媛, 阮敏, 常丽贤, 等. 儿童急性髓系白血病诱导化疗期间血流感染情况分析[J]. 中华儿科杂志, 2021, 59(6): 501-505. Ren YY, Ruan M, Chang LX, et al. Analysis of bloodstream infections in children with acute myeloid leukemia during induction chemotherapies[J]. Chinese Journal of Pediatrics, 2021, 59(6): 501-505. |
| [14] |
湛玉晓, 张俭, 樊彩芳, 等. 儿童急性淋巴细胞白血病化疗后血流感染的病原体分布与耐药变迁分析[J]. 中国当代儿科杂志, 2022, 24(2): 176-181. Zhan YX, Zhang J, Fan CF, et al. Distribution and drug resistance profiles of pathogens causing bloodstream infection after chemotherapy in children with acute lymphoblastic leukemia[J]. Chinese Journal of Contemporary Pediatrics, 2022, 24(2): 176-181. |
| [15] |
巫一立, 余莉华, 林丹娜, 等. 儿童急性白血病多重耐药菌血流感染的临床特征和高危因素分析[J]. 中国实用儿科杂志, 2019, 34(5): 414-418. Wu YL, Yu LH, Lin DN, et al. Clinical features and risk factors analysis in children with acute leukemia complicated with multidrug-resistant bloodstream infection[J]. Chinese Journal of Practical Pediatrics, 2019, 34(5): 414-418. |
| [16] |
黄嘉惠, 叶中绿. 儿童白血病合并多重耐药菌感染的研究进展[J]. 临床荟萃, 2021, 36(2): 188-192. Huang JH, Ye ZL. Progress in childhood leukemia associated with multiple drug-resistant bacterial infections[J]. Clinical Focus, 2021, 36(2): 188-192. |
| [17] |
刘娟, 周璇, 张蕾, 等. 白细胞介素-6、C-反应蛋白和降钙素原对儿童血液肿瘤感染的预测价值[J]. 癌症进展, 2020, 18(20): 2122-2125, 2142. Liu J, Zhou X, Zhang L, et al. Interleukin-6, C-reactive protein and procalcitonin in prediction of pediatric hematological tumor infection[J]. Oncology Progress, 2020, 18(20): 2122-2125, 2142. |
| [18] |
罗增文, 余锋尤, 李彩虹. 大面积烧伤患者深静脉导管引发脓毒血症的影响因素分析[J]. 中国实用医药, 2020, 15(26): 23-25. Luo ZW, Yu FY, Li CH. Analysis of influencing factors of sepsis caused by deep venous catheter in large area burned patients[J]. China Practical Medicine, 2020, 15(26): 23-25. |
| [19] |
国家卫生健康委办公厅医政医管局. 血管导管相关感染预防与控制指南(2021版)[J]. 中国感染控制杂志, 2021, 20(4): 387-388. The Medical Administration and Medical Management Bureau of the General Office of the NHC. Guidelines for the prevention and control of vessel catheter associated infection (2021 Edition)[J]. Chinese Journal of Infection Control, 2021, 20(4): 387-388. |
| [20] |
Nesargi P, Niranjan HS, Bandiya P, et al. Neutrophil volu-me, conductivity and scatter (VCS) as a screening tool in neonatal sepsis[J]. Sci Rep, 2020, 10(1): 4457. |
| [21] |
宋丽丽, 朱莹莹, 管玉洁, 等. 新诊断儿童急性白血病诱导治疗阶段院内感染危险因素分析[J]. 中国实用医刊, 2019, 46(4): 40-42. Song LL, Zhu YY, Guan YJ, et al. Analysis of risk factors of nosocomial infection during induction therapy phase in children with newly diagnosed acute leukemia[J]. Chinese Journal of Practical Medicine, 2019, 46(4): 40-42. |
| [22] |
何琼, 刘科华, 冯振亭, 等. 急性白血病化疗患者肛周感染发生状况及其影响因素[J]. 国际护理学杂志, 2020, 39(19): 3495-3499. He Q, Liu KH, Feng ZT, et al. Perianal infection and its influencing factors in patients with acute leukemia undergoing chemotherapy[J]. International Journal of Nursing, 2020, 39(19): 3495-3499. |
| [23] |
亓欣, 陆爱文. 急性白血病化疗患者并发医院感染的危险因素与护理对策[J]. 国际护理学杂志, 2022, 41(3): 408-412. Qi X, Lu AW. Risk factors and nursing countermeasures for concurrent nosocomial infection in patients with chemotherapy for acute leukemia[J]. International Journal of Nursing, 2022, 41(3): 408-412. |
| [24] |
张晓艳, 何梦雪, 张冰花. 不同营养评价指标在急性淋巴细胞白血病患儿诱导缓解期的临床应用价值[J]. 中国实用护理杂志, 2022, 38(25): 1933-1938. Zhang XY, He MX, Zhang BH. Clinical value of different nutritional evaluation indexes in acute lymphoblastic leukemia pediatric patients during the stage of remission induction[J]. Chinese Journal of Practical Nursing, 2022, 38(25): 1933-1938. |
| [25] |
林嘉乐, 刘亢亢, 储金华, 等. 急性淋巴细胞白血病儿童营养状况与医院感染相关性研究[J]. 中国实验血液学杂志, 2020, 28(3): 767-774. Lin JL, Liu KK, Chu JH, et al. Relationship between nutritional status and nosocomial infection in children with acute lymphoblastic leukemia[J]. Journal of Experimental Hemato-logy, 2020, 28(3): 767-774. |
| [26] |
Loeffen EAH, Brinksma A, Miedema KGE, et al. Clinical implications of malnutrition in childhood cancer patients-infections and mortality[J]. Support Care Cancer, 2015, 23(1): 143-150. |
| [27] |
陈晓文, 侯丽丽, 夏瑞祥. 老年急性白血病患者营养状况与医院感染的相关性研究[J]. 中华老年医学杂志, 2021, 40(7): 895-898. Chen XW, Hou LL, Xia RX. The correlation study between nutritional status and nosocomial infection in elderly patients with acute leukemia[J]. Chinese Journal of Geriatrics, 2021, 40(7): 895-898. |
| [28] |
连敏, 隗玮, 田海军. 高龄老年人医院获得性肺炎合并脓毒症的高危因素及预后分析[J]. 中华老年多器官疾病杂志, 2022, 21(7): 521-525. Lian M, Kui W, Tian HJ. Risk factors and prognosis of hospital-acquired pneumonia complicated with sepsis in very old patients[J]. Chinese Journal of Multiple Organ Diseases in the Elderly, 2022, 21(7): 521-525. |
| [29] |
马红, 宋应明. 急性髓系白血病诱导缓解期并发院内获得性下呼吸道感染的相关因素分析[J]. 中国实用医刊, 2018, 45(15): 93-95. Ma H, Song YM. Analysis of factors associated with acute hospital acquired lower respiratory tract infection in remission with acute myeloid leukemia[J]. Chinese Journal of Practical Medicine, 2018, 45(15): 93-95. |
| [30] |
高晓艳, 田小清, 吕润林, 等. 难治性急性淋巴细胞白血病患儿治疗效果与地塞米松治疗敏感性的关系及耐药机制探讨[J]. 药物评价研究, 2019, 42(9): 1826-1830. Gao XY, Tian XQ, Lv RL, et al. Relationship between therapeutic effect of refractory acute lymphoblastic leukemia and sensitivity of dexamethasone and the mechanism of drug resis-tance[J]. Drug Evaluation Research, 2019, 42(9): 1826-1830. |
| [31] |
张红曦, 李根, 李玲姣, 等. 醋酸泼尼松致急性B淋巴细胞白血病患儿肝损伤1例[J]. 中国药师, 2020, 23(8): 1593-1595. Zhang HX, Li G, Li LJ, et al. Liver injury in a child with prednisone acetate for acute B lymphocytic leukemia[J]. China Pharmacist, 2020, 23(8): 1593-1595. |
| [32] |
Dix D, Cellot S, Price V, et al. Association between corticosteroids and infection, sepsis, and infectious death in pediatric acute myeloid leukemia (AML): results from the Canadian infections in AML research group[J]. Clin Infect Dis, 2012, 55(12): 1608-1614. |



